Senior Employment Services Counselor - Behavioral Health
County of Riverside
Posted: February 13, 2026 (1 day ago)
This job was posted recently. Fresh listings typically have less competition.
Contra Costa County
Health Services - Only
Location
Martinez, California, 94553
Salary
$17,065.92 - $20,743.74
per month
Type
Full Time
More Healthcare & Medical jobs →Closes
Base salary range: $147,649 - $221,900
Typical requirements: Executive-level leadership experience. Senior executive qualifications required.
Note: Actual salary includes locality pay (15-40%+ depending on location).
This job involves leading a team of nurses and staff to manage how healthcare services are approved and delivered in a county health plan, ensuring everything runs smoothly, follows the rules, and helps people get the right care without delays.
It's a leadership role focused on reviewing medical requests, coordinating with doctors and hospitals, and improving patient outcomes in a busy public health setting.
A good fit would be an experienced nurse or healthcare manager who is organized, good at working with teams, and passionate about fair access to quality care for diverse communities.

Contra Costa Health is offering an excellent opportunity for one (1) Health Plan Nurse Program Director within the Contra Costa Health Plan (CCHP) division: Utilization Management (UM)
Contra Costa Health Plan (CCHP) has been serving county residents with their health needs for over 50 years and was the first federally qualified, state-licensed, county-sponsored Health Maintenance Organization (HMO) in the United States.
Established in 1973, CCHP continues to serve as the largest managed care health plan in Contra Costa County, covering over 250,000 residents.
CCHP is committed to ensuring equitable, accessible, and coordinated care for our diverse members. These leadership positions are critical to advancing CCHP’s mission of providing affordable, high-quality healthcare to all.
License Required: Candidates must possess and maintain throughout the duration of employment: a current, valid, and unrestricted Registered Nurse license issued by the California Board of Registered Nursing.
Applicants are required to attach a copy of their license and transcripts to their application.
Education: Possession of a Master's Degree in nursing, hospital or health care administration, or a closely related field, from an accredited college or university.
Experience: Five (5) years of full-time experience, or its equivalent, as a Registered Nurse, Utilization Review Nurse, Discharge Planner, Case Management Nurse, or a Telephone Triage Registered Nurse in a healthcare or managed care setting (e.g.
Preferred Provider Organization, Managed Care Organization, or Health Maintenance Organization), at least one (1) year must have been at a supervisory level.
Substitution: Possession of a Bachelor's Degree in one of the fields noted above plus two (2) additional years of supervisory experience of the type noted above may be substituted for the Master's Degree. There is no substitution for the one (1) year of supervisory experience.
Possession of a Certified Case Manager (CCM) certification issued by the Commission for Case Manager Certification may be substituted for one (1) year of the required experience.
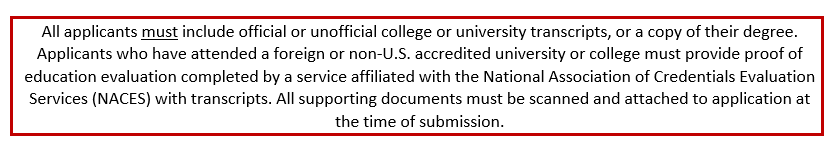
Application Filing and Evaluation: Applicants will be required to complete a supplemental questionnaire at the time of application.
Applications will be evaluated to determine which candidates will move forward in the next phase of the recruitment process.Training & Experience Evaluation: Candidates who clearly demonstrate that they possess the minimum qualifications will have their training and experience evaluated.
The responses to the supplemental questions, at the time of filing, will be evaluated to determine each candidate's relevant education, training, and/or experience as presented on the application and supplemental questionnaire.
(Weighted 100%) For recruitment questions, please contact Health Services Personnel, Recruitment Team at Exams@cchealth.org.
For any technical issues, please contact the Government Jobs’ applicant support team for assistance at +1 855-524-5627.The Human Resources Department may change the examination steps noted above in accordance with the Personnel Management Regulations and accepted selection practices.CONVICTION HISTORYAfter you receive a conditional job offer, you will be fingerprinted, and your fingerprints will be sent to the California Department of Justice (DOJ) and the Federal Bureau of Investigation (FBI).
The resulting report of your conviction history (if any) will be used to determine whether the nature of your conviction conflicts with the specific duties and responsibilities of the job for which you have received a conditional job offer.
If a conflict exists, you will be asked to present any evidence of rehabilitation that may mitigate the conflict, except when federal or state regulations bar employment in specific circumstances.
Having a conviction history does not automatically preclude you from a job with Contra Costa County.
If you accept a conditional job offer, the Human Resources Department will contact you to schedule a fingerprinting appointment.DISASTER SERVICE WORKERAll Contra Costa County employees are designated Disaster Service Workers through state and local law.
Employment with the County requires the affirmation of a loyalty oath to this effect.
Employees are required to complete all Disaster Service Worker-related training as assigned, and to return to work as ordered in the event of an emergency.EQUAL EMPLOYMENT OPPORTUNITYIt is the policy of Contra Costa County to consider all applicants for employment without regard to race, color, religion, sex, national origin, ethnicity, age, disability, sexual orientation, gender, gender identity, gender expression, marital status, ancestry, medical condition, genetic information, military or veteran status, or other protected category under the law.
Check your resume before applying to catch common mistakes